Simulation for training purposes was born in the aeronautical field around the ’60s for the safety training of flight pilots. In a short time this tool has found wide use in all those industrial sectors (such as the military, nuclear or chemical industries) where complex and high-risk procedures are carried out daily. An intense preparation of operators is required in these sectors and can be obtained in controlled environments where even very risky scenarios can be faced without any negative impact on the environment or on the person, thus allowing “learning by error”.
There is also a growing interest in the medical field in the use of simulation as a training method for health personnel. The reasons for this interest are to be found in the need to guarantee the patient a high quality of treatment while minimizing the possibility of error. In the last twenty years, also following a British Medical Journal report denouncing medical error as the third cause of death, there has been a growing attention to patient protection. In this context, simulation as a training method allows doctors and nurses to improve their skills and technical abilities, guaranteeing a standard of safety and reducing public health costs.
Simulation tools now also find clinical application in the preoperative planning of complex surgical interventions. In these cases, in fact, the operator can use anatomical physical replicas to study and test the best intervention strategy before entering the operating room. Thanks to the planning of the intervention and the three-dimensional visualization of the anatomy, unconventional access routes to the injured anatomical region can be identified, allowing a minimally invasive approach with regard to the surrounding healthy tissues.
Simulation in neurosurgery
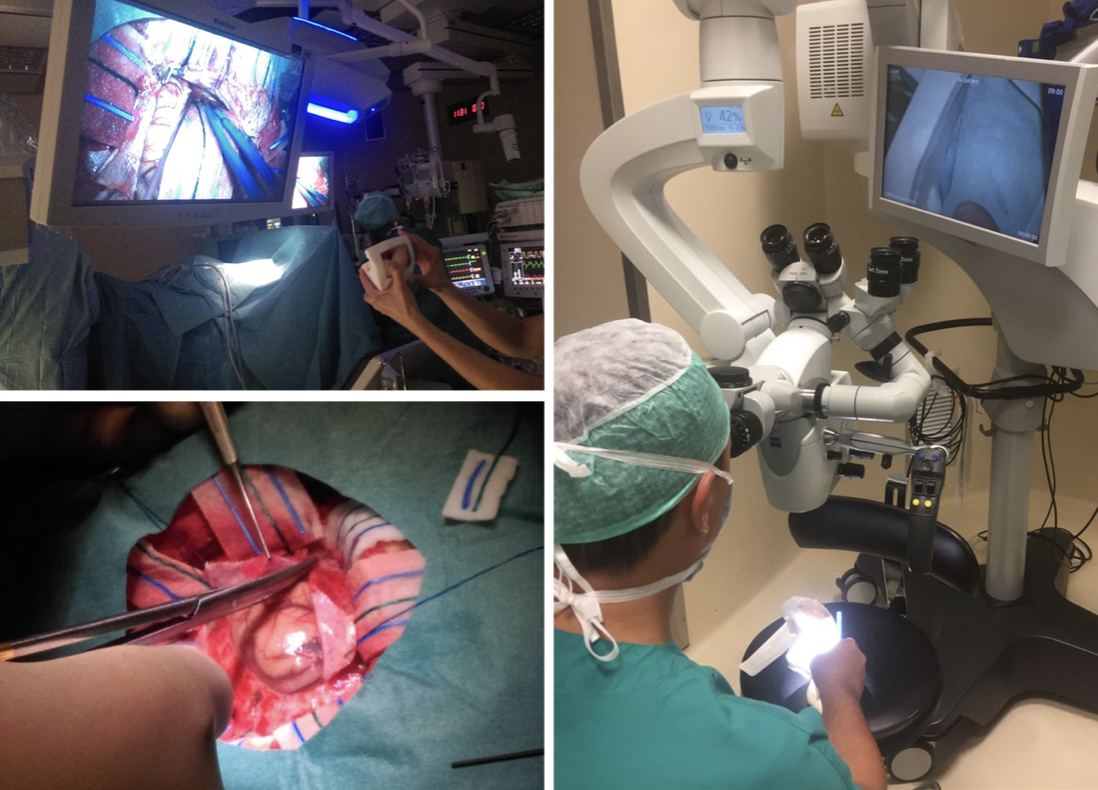
In neurosurgery, preoperative simulation can be used, for example, in brain tumor removal interventions. Brain tissue resection is a procedure that requires high precision by the neurosurgeon so as not to damage the primary areas of the brain and thus avoid irreversible neurological deficits that can prevent a regular social life.
Preoperative planning is a crucial step in the neurosurgeon’s preparation for surgery as it defines the access route to the tumor, allows the patient’s anatomical geometry to be memorized and a proprioceptive spatial map to be created. In traditional clinical practice, planning begins with the evaluation of medical images, a critical moment for successful surgery. During this phase, in fact, the expert operator is able to mentally reconstruct the three-dimensional geometry of the site of interest on which to plan the surgery; it often happens that due to fear of overestimating the area to be removed, the neurosurgeon unconsciously tends to choose a more conservative approach that involves a lower risk of damage to primary brain areas on one hand, but on the other the risk of not removing all the diseased tissue.
The introduction of the 3D printer in medicine has revolutionized clinical practice, allowing the exact physical reproduction of complex and geometrically difficult anatomical shapes with traditional production techniques. In this way, the surgeon can handle a physical replica of the anatomy of interest, allowing the tactile exploration of the site to be operated, achieving greater awareness of spatial volumes and relationships and improving hand-eye coordination.
From medical images to 3D model
The production process of the three-dimensional anatomical model involves:
- the acquisition of data by diagnostic imaging techniques
- image segmentation
- the use of three-dimensional modeling software
- 3D printing
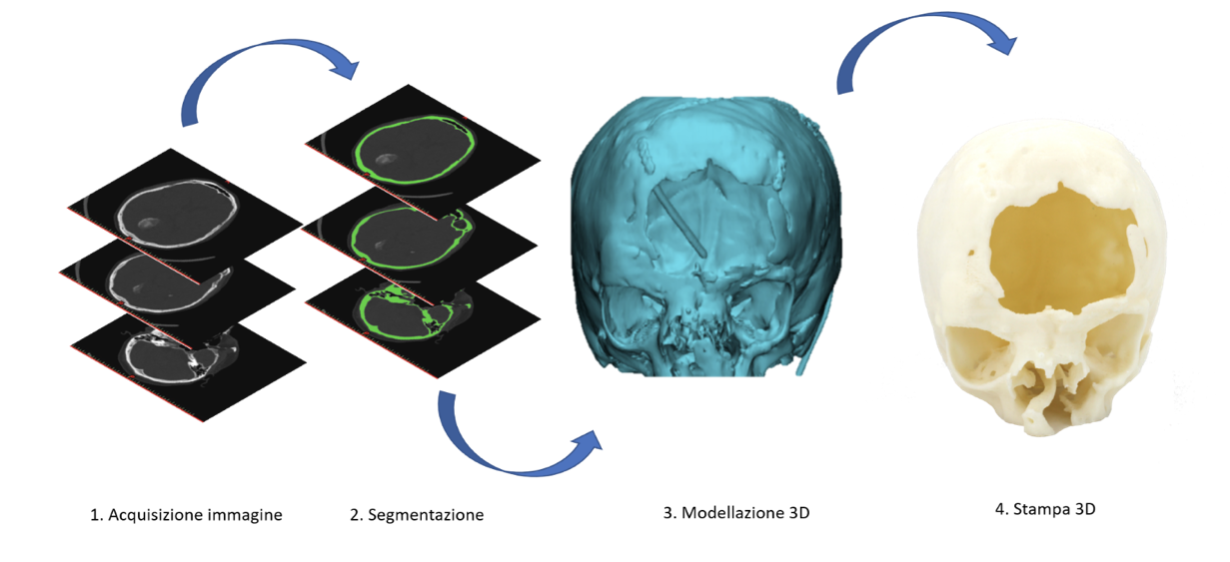
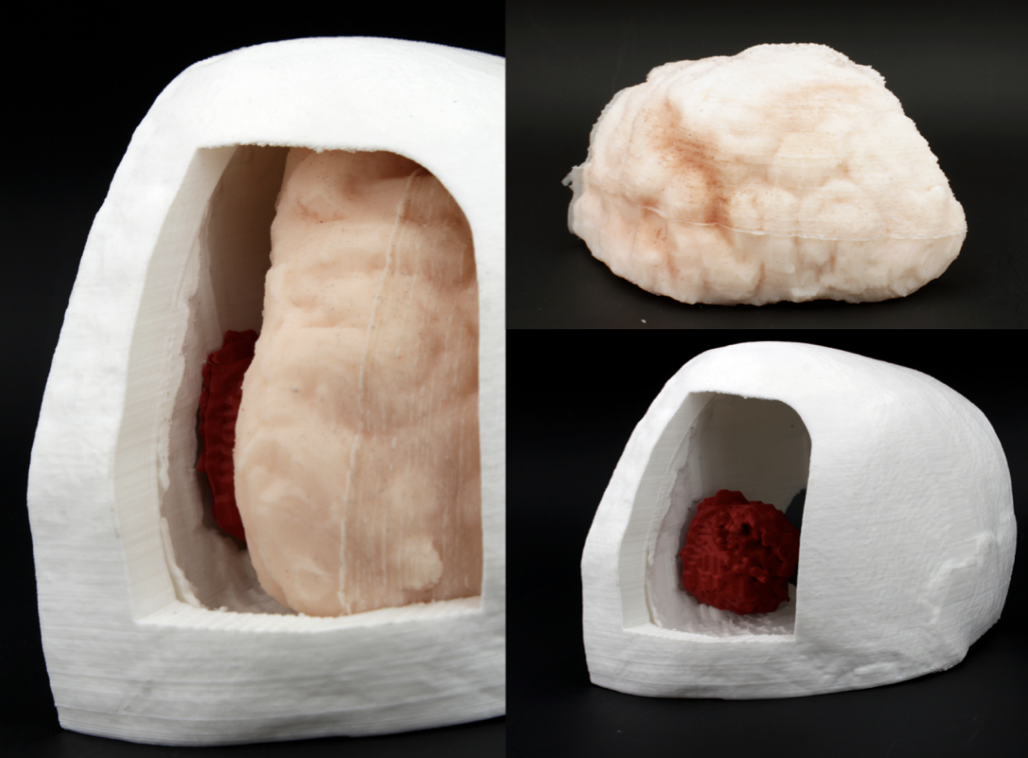
The image acquisition phase is of considerable importance: the quality of the data acquired also determines the quality of the final product and guarantees the reproduction of a realistic anatomy faithful to that of the subject in question. In order to isolate the region of interest, a segmentation or division of the image into regions corresponding to structural units is performed. Due to the complexity of the human anatomy, this process requires trained personnel with specific skills. The result of the segmentation is then processed with special 3D modeling software, generating a digital replication of the anatomical region of interest. 3D printing allows transition from the digital model to the physical model, which is provided to the neurosurgeon. Specifically, the simulator can be produced through direct printing, generally with plastic materials, of the anatomical replica or through indirect printing, or through the production of moulds (negatives of the anatomy to be replicated) in which silicone rubbers are cast that have mechanical characteristics consistent with the tissues to be simulated.
The T3DDY experience and clinical cases
Within the joint laboratory T3DDY, a collaboration between Meyer Children’s Hospital and the Industrial Engineering Department of the University of Florence, neurosurgical simulators for preoperative planning have been realized thanks to the use of 3D printing.
One of the simulators realized is related to the planning of the intervention of a sixteen-year-old girl suffering from a benign tumor at the base of the skull. The position of the tumor was compromising the function of the optic nerve and required the study of an alternative access route to the diseased tissue to preserve the nerve. 3D technology allowed the simulation and preoperative planning of the surgery by creating a physical model that was highly faithful to the patient’s anatomy (skull, tumor and optic nerve).
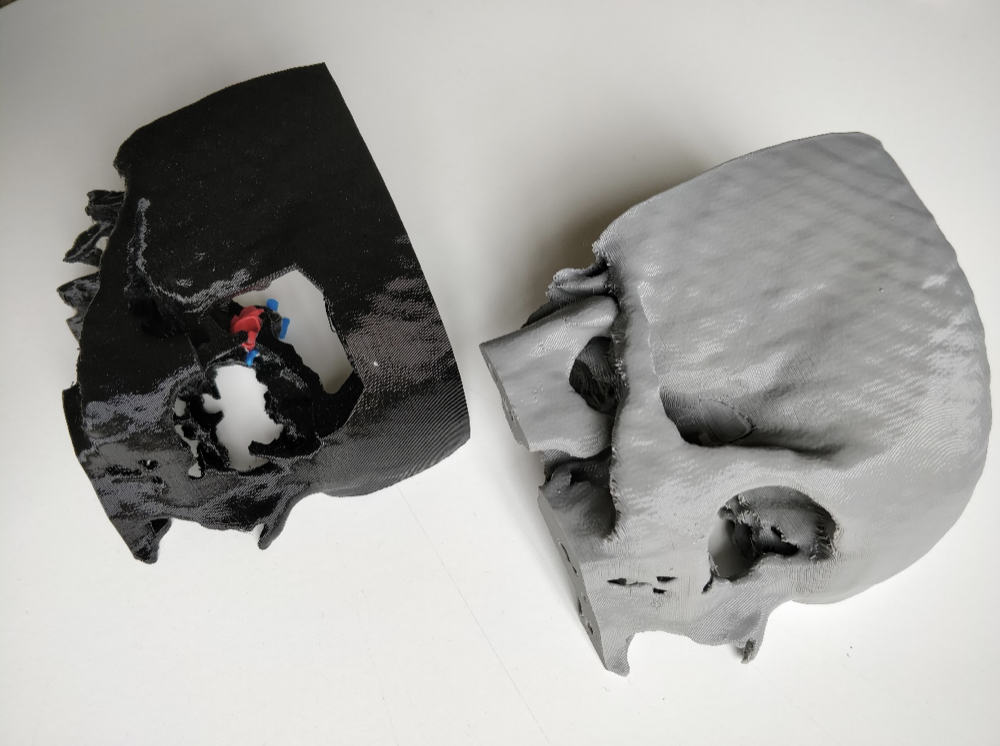
Thanks to the careful study of physical replication, it was possible to identify an optimal trajectory for the removal of the tumor, which involved the removal of the orbital bone, making the surgery minimally invasive and at low risk of brain injury. Another simulator was produced for the surgery of a patient with meningioma at the temorium level. In this case the particular position of the tumor required an accurate study of the geometry and spatial location of the meningioma positioned near a venous sinus.
The simulator for the preoperative planning of this case required the direct printing of the skull and tumor and the realization of the brain with silicone materials cast inside a mould obtained with 3D printing technology.
The simulator, prior to surgery, was observed under the microscope allowing the physician to become familiar with the surgical field and the spatial relationships of the tissues present.
Conclusions
3D printing technology within the medical simulation landscape is revolutionizing clinical practice by enabling accurate replication of patient-specific human anatomy while implementing a personalized medical approach. This technology can therefore be considered a valuable tool in neurosurgery for the resolution of complex clinical cases. In fact, the use of neurosurgical simulators allows study, simulation and the performance of increasingly less invasive surgical procedures. This leads to a reduction in operating times, patient admission times and therefore costs for the healthcare system.

